Facet Joint Injections
- Home
- Facet Joint Injections
Facet Joint Injections for Back and Neck Pain in Singapore
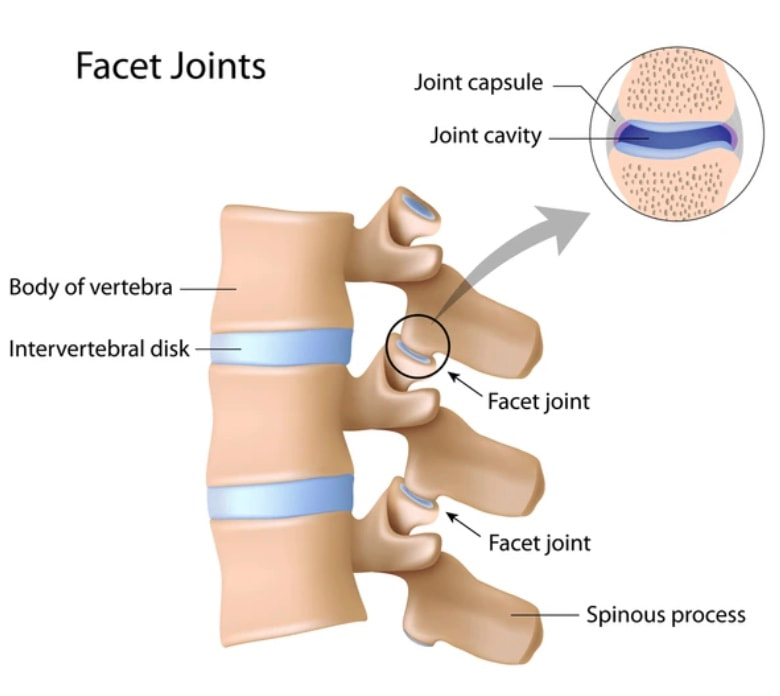
Facet joints, also known as zygapophyseal joints, are small, paired joints that connect the vertebrae in your spine. They provide structure and enable controlled movement, allowing the spine to bend and twist. Located on each side of the vertebrae, facet joints link the superior articular process of one vertebra to the inferior articular process of the vertebra above or below.
These joints are lined with cartilage, which cushions the surfaces, and are filled with synovial fluid that helps with lubrication. They are enclosed in a joint capsule, providing both stability and flexibility. The alignment and orientation of facet joints differ throughout the spine, contributing to the varying range of motion in the neck, upper back, and lower back regions.
Facet joints are essential for supporting a wide range of spinal movements like flexion, extension, and rotation. However, they can also become a source of pain and dysfunction when conditions such as facet joint syndrome, osteoarthritis, or spinal stenosis cause inflammation, degeneration, or injury.
How Is Facet Joint Pain Diagnosed?
Facet joint pain typically manifests as a localized ache or sharp discomfort, often felt in the lower back (lumbar area) or neck (cervical area), depending on which facet joints are affected. This pain may radiate to surrounding areas like the buttocks, hips, or shoulders.
Diagnosing facet joint pain generally involves a combination of medical history, a physical examination, and imaging studies (X-rays, MRIs, or CT scans). However, it’s important to note that radiographic findings may show facet joint degeneration or arthritis even in patients who do not have symptoms. The most reliable way to confirm facet joint pain is through a diagnostic medial branch block, a procedure that helps determine whether the facet joints are the primary pain source.
How Is Facet Joint Pain Treated?
When facet joint pain is first experienced, conservative treatments are typically recommended. This may include non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or physical therapy to enhance mobility, strengthen muscles, and alleviate discomfort.
If conservative treatments do not provide adequate relief and facet joint dysfunction is suspected, a diagnostic medial branch block can be performed. This procedure helps confirm the facet joints as the source of the pain.
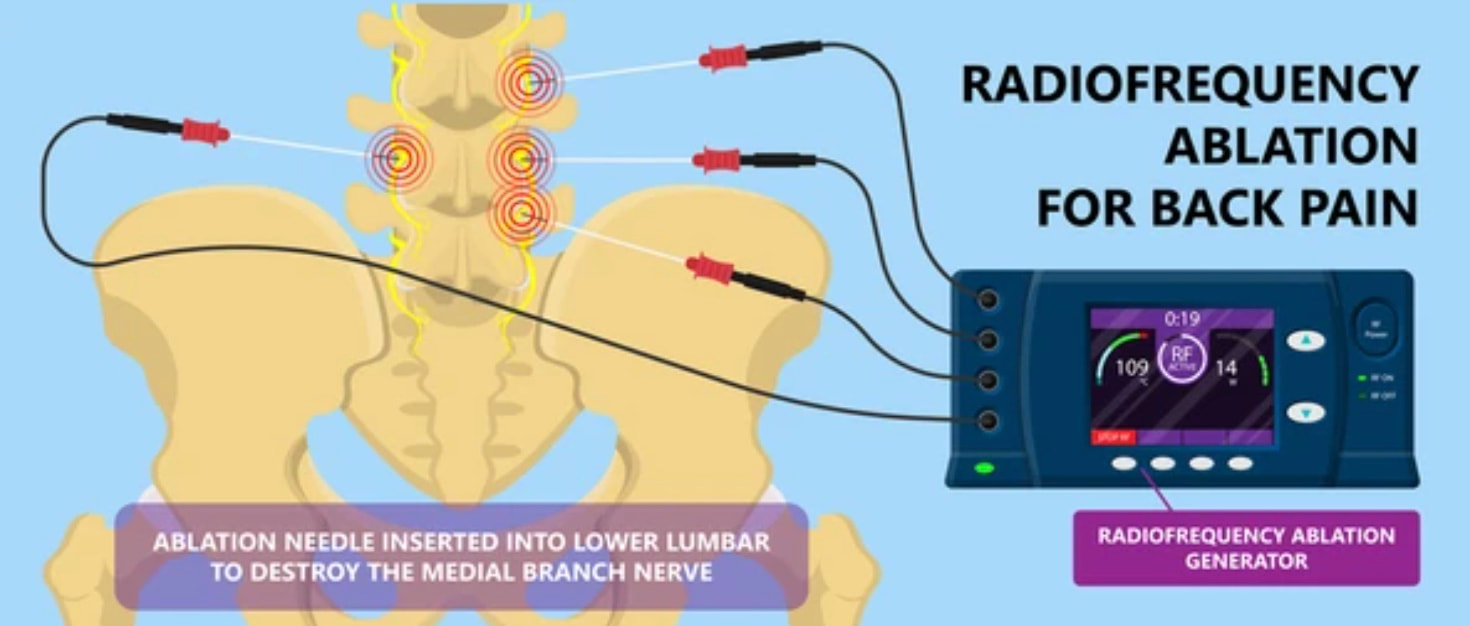
Once facet joint involvement is confirmed, your doctor may suggest a more targeted treatment called radiofrequency ablation (RFA). RFA involves using heat to disrupt the nerves transmitting pain signals from the facet joints, providing longer-lasting pain relief.
What Is a Facet Joint Injection?
A facet joint injection is a therapeutic procedure designed to treat chronic back or neck pain originating from the facet joints. It is a powerful non-surgical back pain treatment for conditions like facet joint arthritis, where inflammation within the joints causes significant discomfort and stiffness.
During the procedure, a mixture of local anaesthetic for immediate numbing and a long-lasting corticosteroid to reduce inflammation is injected directly into the targeted joint capsule. This treatment, performed under imaging guidance for precision, aims to provide significant pain relief that can last for several weeks or months.

Differences Between Medial Branch Block and Facet Joint Injection
| Aspect | Medial Branch Block (MBB) | Facet Joint Injection (FJI) |
| Primary Goal | Diagnostic: Confirms the source of pain | Therapeutic: Relieves pain and inflammation |
| Injection Target | Nerves outside the joint | Directly inside the joint capsule |
| Medication | Local anaesthetic only. | Anaesthetic + Corticosteroid |
| Relief Duration | Short-term (a few hours to days) | Longer-term (weeks to months) |
| Next Step | If successful, Radiofrequency Ablation | Can be repeated for ongoing relief |
What Are the Potential Side Effects of Facet Joint Injections?
Facet Joint Injections are very safe, especially when performed by a specialist under image guidance. Most side effects are mild and temporary, such as:
- Soreness or mild bruising at the injection site.
- A temporary increase in pain before the medication takes full effect.
Serious complications are rare. Our team will discuss all potential risks with you before the procedure.
Why Choose Our Clinic for Facet Joint Injection Treatment in Singapore?
Living with chronic pain is challenging, but a precise diagnosis from a dedicated specialist is the first step toward relief. Dr Christopher Liu is an expert neck and shoulder pain specialist who also provides leading sciatica treatment in Singapore. He uses advanced diagnostic tools like the medial branch block to pinpoint the exact source of your discomfort, ensuring a targeted and effective plan.
For a premier facet joint injection in Singapore, trust Dr Liu’s comprehensive approach. He is committed to creating a personalised treatment plan to help you find lasting relief. Contact us today to schedule your consultation!
If you believe you may have an annular tear or suffer from chronic low back pain, schedule an appointment with the specialists at Alleviate Pain Clinic, located at Farrer Park Hospital, Singapore. Our Doctors can provide a comprehensive evaluation and tailor a treatment plan to help you manage and overcome your pain effectively.
Go To Top
Chat with us

